A team led by scientists at the University of Illinois at Urbana Champaign (UIUC) tracked the rise and fall of sars-cov-2 in the saliva and nasal cavities of people newly infected with the virus. This study is the first study to track the time of acute covid-19 infection by repeated sampling and compare the results of different test methods.
The research results were published in nature microbiology.
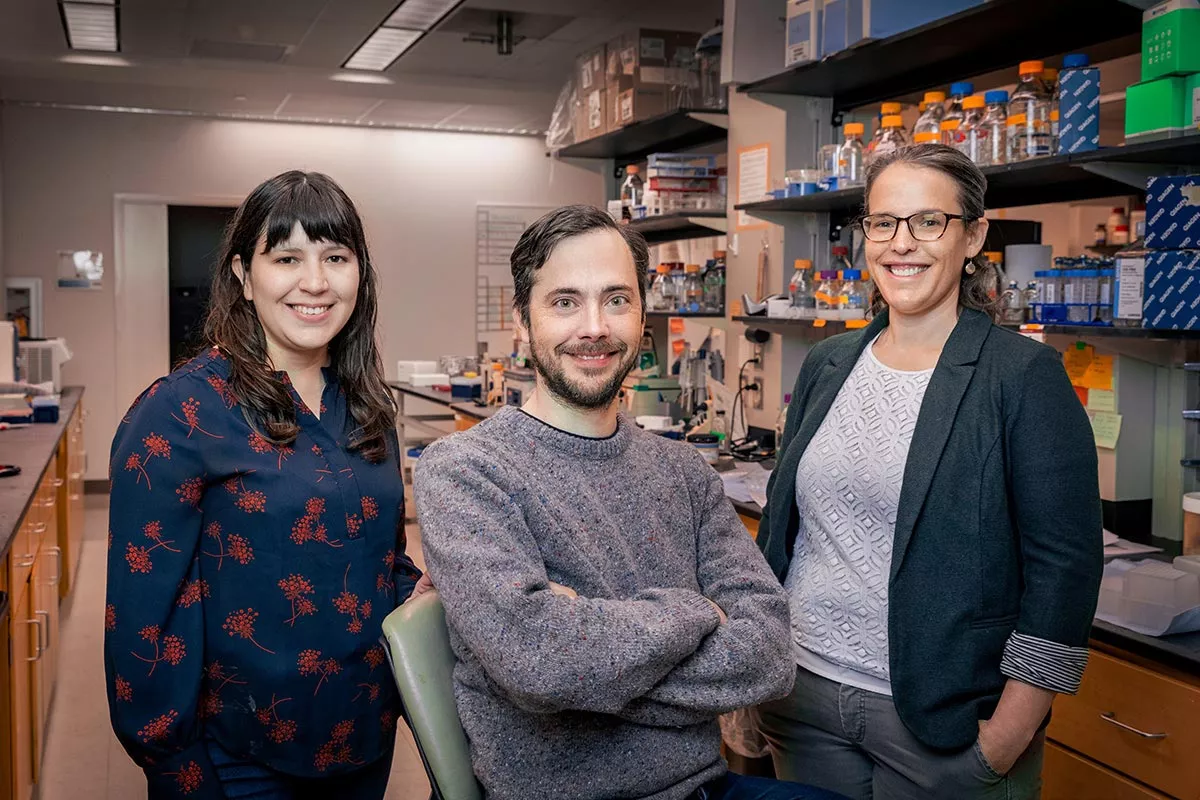
"We have captured the most complete, high-resolution, quantitative picture of how sars-cov-2 replicates and falls off in the human body during natural infection. There is no other similar data. This study reveals several aspects of infection that are important for public health and basic biology," said Christopher B. Brooke, a professor of Microbiology at the University of Chicago. He led the study with Pamela P. Martinez, Professor of Microbiology and statistics, and Rebecca L. Smith, Professor of pathobiology.
The study is based on the shield: target, test, tell initiative, the covid-19 response plan of the University of Illinois. The program began testing staff, students and faculty twice a week in the fall of 2020. Researchers in Illinois realized that the test data could be a treasure house of information about the infection process: such as the replication rate of different sars-cov-2 variants and the ability of individuals to clear the infection.
The National Institutes of Health funded comparative PCR tests - amplification and detection of viral RNA, rapid antigen testing - to find virus related proteins. This funding makes other aspects of the study possible.
Starting within 24 hours of the initial positive test, the team collected nasal and saliva samples from adults who tested positive for covid-19 infection every day. The 60 participants in the study ranged in age from 19 to 73. The study tracked everyone for up to 14 days.
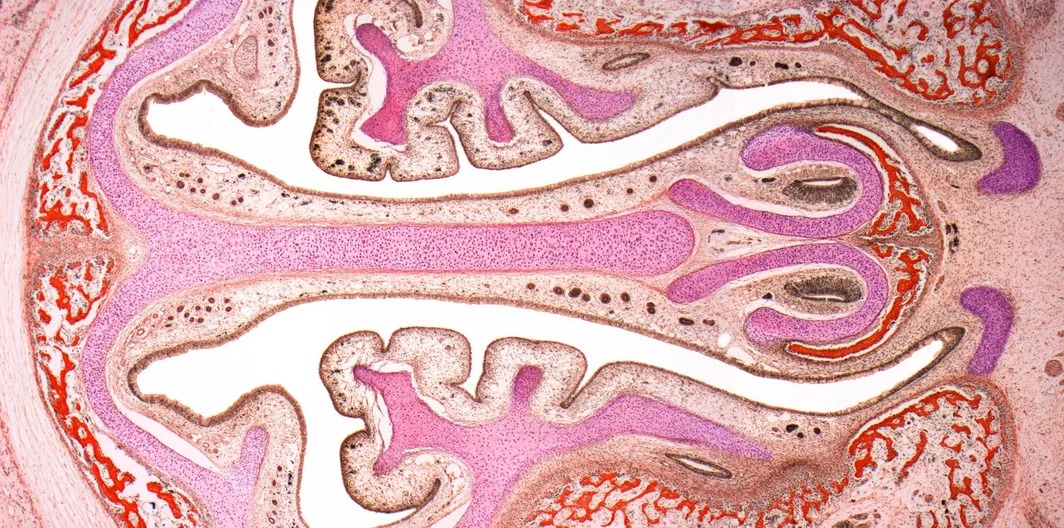
Brooke said that determining how long infected people may shed the virus in their saliva or nasal cavity is the key to understanding how the virus spreads and persists in people. To do this, the team also used a virus culture method to measure the shedding of infectious viruses in their samples. "Just because you see the signal of the virus through PCR or antigen test does not mean that there is indeed a live virus that can replicate and fall off and spread to others."
Ruian Ke, a collaborator of Los Alamos National Laboratory and the first author of the paper, used various mathematical models to help the research team understand how the data reflect the potential infection process and identify the factors affecting the infection process.
The work showed that some people shed the live virus in only a day or two, while others continued to shed the virus for nine days.
"Based on this finding, we predict that those who shed the virus for more than a week will have a greater risk of transmission than those who can detect the live virus in only a day or two," Brooke said.
Martinez said: "this is a very critical finding. People have observed that virus transmission is heterogeneous, but most people attribute these differences to personal behavior. We assume that super communicators are less cautious or contact more people. This shows that the internal dynamics of infection also plays an important role."
The researchers also found that the viral genome load - which can be detected by PCR - peaked earlier in saliva samples than in nasal swabs.
This suggests that saliva may be a superior sampling point for early detection of infection, the researchers wrote.
Scientists did not see significant differences in the infection dynamics of the early circulating variant and alpha variant of sars-cov-2 virus. This suggests that the higher transmission of alpha variants cannot be explained by higher viral load or delayed clearance, the researchers noted.
The team saw no meaningful link between people's symptoms and the process of infection. Brooke points out that while it is generally believed that people with more symptoms may be more infectious, this may not always be true. It is worth noting that the significance of this part of the study may be limited because all participants in the study either had no symptoms or mild symptoms and no one was hospitalized.
"Overall, this study helps explain why some people are more likely to spread sars-cov-2 than others," Brooke said.